A crucial health alert for Andhra Pradesh and Palnadu: Understand Melioidosis (Whitmore’s Disease), symptoms, transmission, high-risk groups, and the complete two-phase antibiotic treatment. Essential awareness following reported cases in the region.
Why Andhra Pradesh Is on Alert: Understanding Melioidosis
Public health officials across Andhra Pradesh, especially in Palnadu District, are sounding the alarm over a silent but dangerous threat, Melioidosis, a severe bacterial infection often mistaken for common fevers.
Nicknamed The Great Mimicker, Melioidosis hides behind symptoms that resemble dengue, tuberculosis, pneumonia, and even routine viral fevers. This makes early diagnosis difficult,a nd delays can turn deadly.
The Palnadu Connection: Why This District Matters
Melioidosis is caused by the soil-dwelling bacterium Burkholderia pseudomallei, which thrives in warm, wet environments found widely across coastal and agricultural belts of AP.
Recent Local Case
A confirmed Melioidosis case was recently reported from Davupalli Thanda in Veldurthi Mandal, Palnadu District, prompting immediate public health action.
Government Response
Authorities have launched:
- Intensive fever surveys
- Sanitation and disinfection drives
- Water quality testing across affected villages
- Awareness campaigns targeting farmers and diabetic patients
The message is clear: Early awareness can save lives.
How Melioidosis Spreads: Not Person-to-Person, but Through the Environment
Melioidosis does not spread like the flu or COVID-19.
You contract it from contaminated soil or water, especially after rains, floods, or while working in fields.
Major Transmission Routes
- Skin contact: Cuts, cracks, and wounds exposed to muddy water or wet soil
- Inhalation: Breathing in contaminated dust or droplets during storms or heavy winds
- Ingestion: Drinking unchlorinated groundwater
The #1 Risk Factor: Diabetes
People with diabetes mellitus are at the highest risk of severe or fatal Melioidosis.
AP and Telangana have some of India’s highest diabetes prevalence rates, making awareness even more critical.
Also Read: 7 Smart Habits To Manage Diabetes Naturally Without Stress
Other High-Risk Groups
- Individuals with chronic kidney or liver disease
- People with chronic lung conditions
- Heavy alcohol consumption
- Elderly individuals exposed to agricultural environments
Symptoms of Melioidosis: What You Should Never Ignore
Symptoms usually appear 1 to 21 days after exposure, but can sometimes take months.
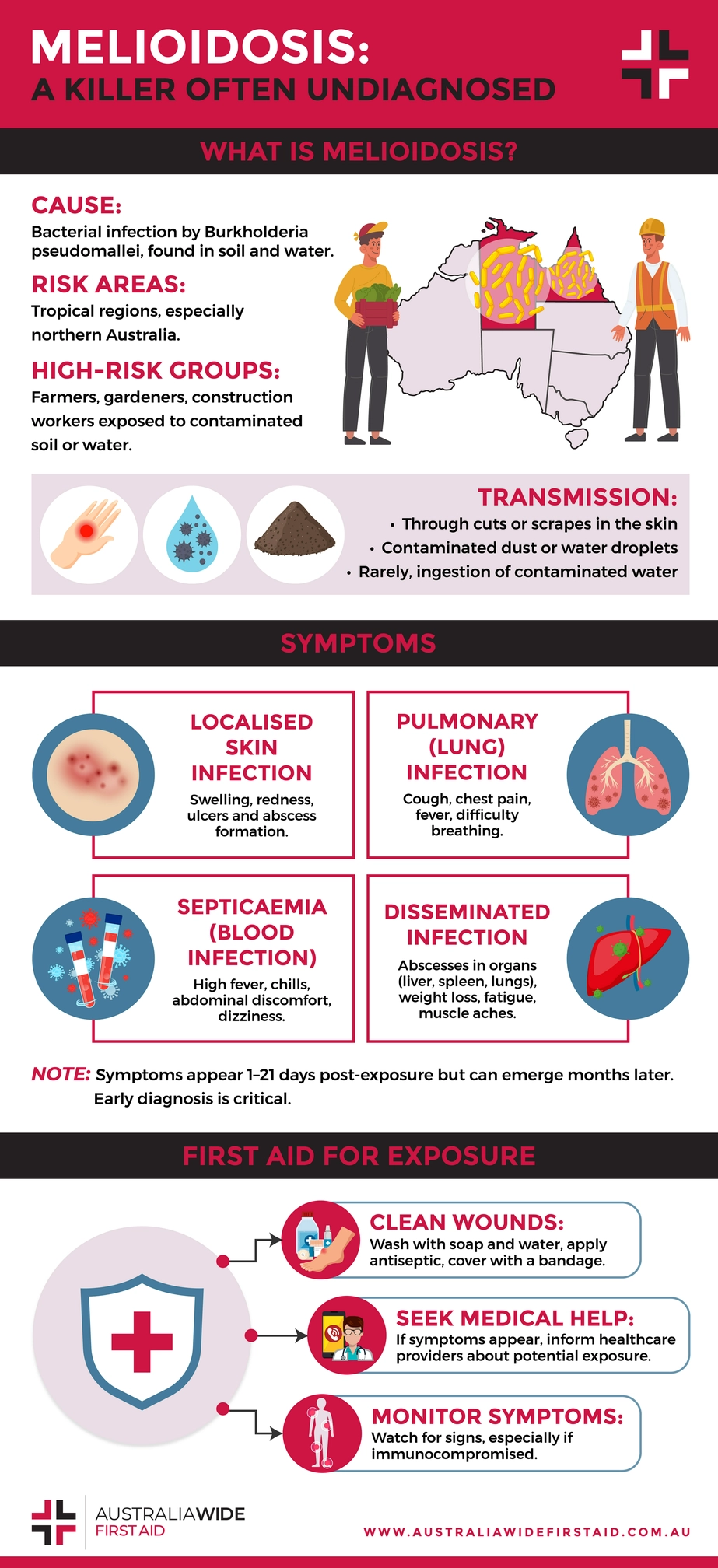

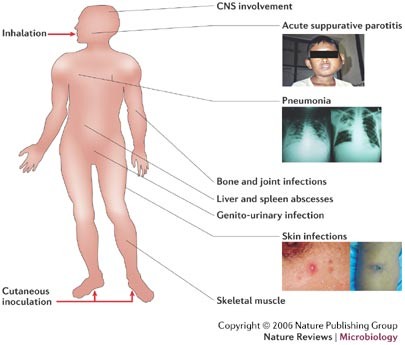
1. Localised Skin Infection
- Persistent skin ulcer
- Abscess filled with pus
- Redness or swelling at the wound site
2. Lung Infection (Most Common Form)
- Sudden high fever
- Severe cough (with or without sputum)
- Chest pain, difficulty breathing
- Mimics pneumonia or tuberculosis
3. Bloodstream Infection (Sepsis)
- Rapid fever spikes
- Extreme weakness
- Confusion or altered mental state
- Can lead to septic shock — a medical emergency
4. Disseminated Infection
- Abscesses in the liver, spleen, and prostate
- Chronic fever that doesn’t respond to routine antibiotics
If you have diabetes and develop a fever after exposure to wet soil or muddy water, alert your doctor immediately.
Treatment: The Two-Phase Antibiotic Cure That MUST Be Completed
Melioidosis is treatable — but only with a strict, two-stage treatment plan.


Phase 1: Intensive IV Therapy (Hospitalised Treatment)
- Duration: 10–14 days (longer if severe)
- Medications: Ceftazidime or Meropenem
- Purpose: Control life-threatening infection
Phase 2: Eradication Therapy (Oral Antibiotics)
- Duration: 3–6 months
- Medication: Trimethoprim-Sulfamethoxazole (Co-trimoxazole)
- Purpose: Kill dormant bacteria & prevent relapse
Stopping antibiotics early is the #1 reason for relapse. Complete the entire course.
Prevention Tips: Especially for Farmers & Families in Rural AP
Cover Wounds
Always use waterproof dressings before entering fields or flood-affected areas.
Wear Protective Gear
- Waterproof boots
- Rubber gloves
- Avoid walking barefoot in wet soil
Keep Diabetes Under Control
High sugar levels reduce immunity and increase infection severity.
Drink Safe Water
Avoid unchlorinated bore water; boil water during monsoon seasons.
Frequently Asked Questions:
Q1. Is Melioidosis contagious?
No. Melioidosis rarely spreads from person to person. The bacteria live in soil and water.
Q2. Who should get tested for Melioidosis?
Anyone with:
- Fever for more than 5 days
- Pneumonia not improving with routine antibiotics
- Skin abscess that doesn’t heal
- Diabetes + exposure to muddy fields
Q3. How is Melioidosis diagnosed?
Through culture tests of blood, sputum, urine, or pus to identify Burkholderia pseudomallei.
Q4. Is Melioidosis new in Andhra Pradesh?
No. It has existed for decades, but diagnosis and reporting have improved, helping save more lives.
Q5. Can Melioidosis be fatal?
Yes, if untreated. But with correct antibiotics and full 3–6 month treatment, recovery rates are high.
Conclusion
Melioidosis may not be widely known, but its impact can be serious, especially in regions like Palnadu, where agricultural exposure and monsoon cycles increase risk. Early detection, strong public awareness, and complete antibiotic therapy are the strongest shields against this “Great Mimicker.”










Leave a Reply